The cornea is the clear front window of the eye. Like windows, it can obscure light or make seeing through it difficult when damaged – such as through scars or swelling.
Disease and injury may cause such damage, which then leads to the cornea blocking or distorting light. The result can be blurred or impaired vision.
Some of the more common corneal issues can be managed with eye drops, medication, or minor procedures. However, there are cases when these treatments can no longer address the issue.
In that case, a cornea transplant or cornea repair surgery may be required. In this article, we explain what patients may expect from this intervention and what key considerations are involved.
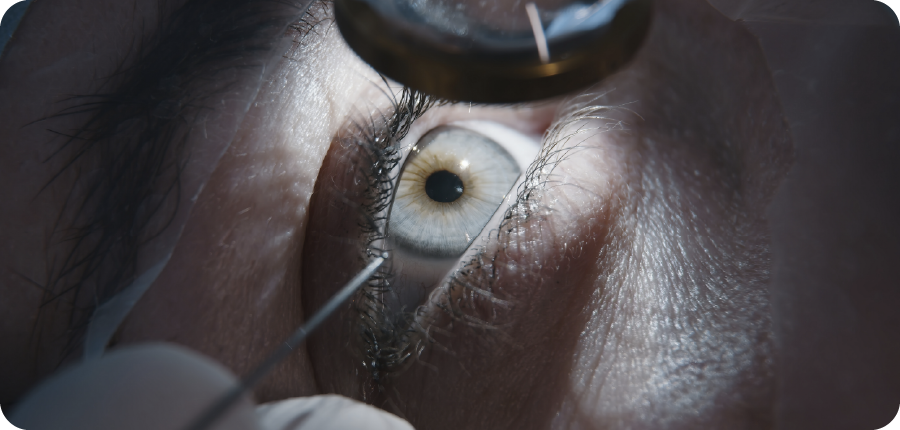
The cornea transplant is also called keratoplasty. This surgical procedure requires an eye surgeon to replace diseased or damaged corneal tissue with healthy donor tissue.
The donor tissue comes from a certified eye bank. By using it, the surgery aims to:
Corneal transplants are among the more common forms of human tissue transplantation. Some studies even report 90% graft survival rates in the first five years post-transplant.
However, outcomes of a cornea transplant may still vary. Many factors can cause variance, from the patient’s underlying eye condition to overall eye health, and even adherence to post-surgery care instructions.
Patients must discuss potential results and risks on an individual basis with their ophthalmologist. No surgical procedure can guarantee specific results.

A corneal transplant is often considered under these conditions:
Examples of conditions requiring surgery are as follows:
Note that repeat procedures may be required for patients with previously rejected or failed corneal grafts.
Common symptoms indicating advanced corneal damage are the following (but a doctor is still required for proper diagnosis):

These are the general types of cornea transplants performed today:
1. Anterior Lamellar Keratoplasty (ALK)
Also known as Deep Anterior Lamellar Keratoplasty (DALK), this procedure replaces the front corneal layers (stroma) while preserving the patient’s own endothelium. It is typically used for diseases that do not affect the innermost corneal layer, such as keratoconus or anterior scars.
2. Endothelial Keratoplasty (EK)
Endothelial keratoplasty targets only the innermost layer of the cornea, called the endothelium. By keeping the outer corneal layers intact, this technique allows for smaller incisions, faster recovery, and a lower risk of graft rejection.
3. Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK)
DSAEK is a type of EK where a thin layer of donor tissue containing the endothelium and part of the stroma is transplanted. The use of automated instruments helps ensure precision, promoting quicker healing and improved visual outcomes compared to older full-thickness grafts.
4. Descemet’s Membrane Endothelial Keratoplasty (DMEK)
DMEK refines the EK approach by transplanting only the donor Descemet’s membrane and endothelial cells. Because the graft is extremely thin and closely matches natural anatomy, it often delivers the sharpest visual results and the lowest rejection rates among corneal transplant methods.
5. Artificial Cornea Surgery
When patients are not suitable candidates for standard human donor corneal grafts, artificial cornea devices are employed. The two main subtypes are the following:
Corneal surgery may also be paired with the supplemental procedure of artificial iris surgery. It can improve both visual function and cosmetic appearance in certain cases.

Patients need a full eye examination with an ophthalmologist, who will conduct tests like slit lamp examinations and corneal topography. Medical clearance will also be necessary to ensure fitness for the surgery.
A patient's doctor should be able to provide details on the risks and benefits of the surgery. The anticipated recovery times and alternative treatments should be discussed as well.
Corneal transplant surgery is most often performed as a day surgery procedure under local anaesthesia with sedation. However, general anaesthesia may be used in some cases too.
The surgeon removes the diseased corneal tissue, and the healthy donor tissue is then shaped to fit and secured to the area with fine stitches or held in place through an air bubble in the eye.
The operation often takes one to 2 hours.
A protective eye shield is often applied following the procedure. Most patients can be discharged on the same day, with clear instructions from their doctors on recovery and medication.

Recovery timeframes depend on a variety of factors. Most patients will see initial healing in the first few weeks, with full visual rehabilitation taking several months.
Patients are often prescribed steroid drops for months or years. These are designed to suppress the body’s immune system and thus prevent graft rejection.
Antibiotic drops are often prescribed in the initial phase too, to reduce infection risk.
Patients will be asked to avoid rubbing or touching the eye for the first few weeks. Activities that may strain it are also recommended against, including heavy lifting or sports.
The patient will also need to sleep with a protective eye shield for safety for a short period.
Frequent follow-ups will be scheduled with the ophthalmologist to ensure that the doctor can monitor the graft and manage any inflammation.
If the graft was sutured or stitched on, the stitches may remain in place for months. The doctor will indicate when to remove them if needed.
All surgeries carry potential risks. The most serious and common risk for this procedure is the allograft rejection episode.
This is when the patient’s immune system attacks the donor tissue. Rejection rates vary by procedure and patient risk; acute rejection episodes can occur and are an important reason for close follow-up.
Other possible complications are infection, astigmatism (which may be caused by stitch tension or uneven graft healing), and graft failure, where the donor tissue loses vision clarity.
Patients must be vigilant for symptoms of rejection or complications:

The corneal epithelium can regenerate, but deeper stromal scarring or irreversible endothelial cell loss usually will not clear on its own and may require surgical intervention.
Hence, even a minor delay in treating a post-op complication may lead to graft failure. Earlier action may improve the chances of saving a corneal graft from permanent failure.
This is why fast action, adherence to post-op recovery instructions, and regular follow-ups matter to patients’ outcomes.
If you believe you are considering or believe you need a cornea transplant, book a consultation with our ophthalmologists at ERS Suntec City.
We can provide a comprehensive evaluation to understand if cornea repair surgery or cornea transplant is suitable for your condition.